The pelvis is the region of the body intermediate to the abdominal cavity and the lower limbs, including the pelvic girdle. The pelvic girdle surrounds the pelvis and is part of the appendicular skeleton. The pelvic girdle is made up of the right coxal bone, left coxal bone, and the sacrum. Also made up of three bones is the coxal bone, the most lateral aspects of the pelvic girdle, formed by the fusion of the ilium, ischium, and pubis. Formed by the fusion of five sacral vertebrae is the sacrum, the most posterior portion of the pelvic girdle. The most anterior aspect of the pelvic girdle is the pubic symphysis, joining the two coxal bones.
Although there are similarities among pelvic girdles, not all pelvic girdles are made equal. The male and female pelvic girdles, as a particular focus, are different in many ways and these differences are typically used when identifying the sex of skeletal remains. The general structure is thick and heavy in males, but thin and light in females. Superior to the pelvic inlet is the greater pelvis which is deep in males, yet shallow in females. Another difference is seen in the lesser pelvis, the region between the pelvic inlet and pelvic outlet, which is narrow and deep with a tapering shape in males and is wide and shallow with a cylindrical shape in females. Also, the pelvic inlet is heart-shaped and narrow in males, leading to a relatively small pelvic outlet while the female pelvic inlet is oval-shaped and wide in females.
The differences between the male and female pelvic girdles are numerous due to the child-bearing function in females. The pubic arch is the space between the junction of the inferior rami of the iscium and pubis on the left side and the same on the right side. Expectedly so, the pubic arch of the male is narrower than that of the female as is the greater sciatic notch. Also, the obturator foramen is of a round shape in males and oval in females. Finally, in terms of the acetabulum, it is larger in males than in females. Some of the differences between the pelvic girdles of males and females, as with the greater pelvis, can be attributed to the greater muscle mass of males in relation to females.

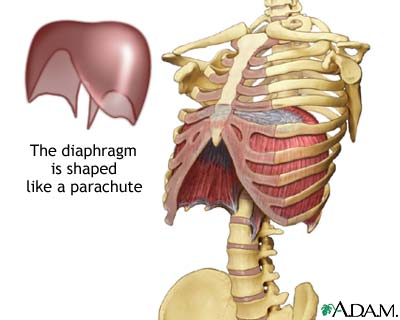
Within the lesser pelvis of both males and females is the pelvic diaphragm, separating the pelvic cavity from the perineum. Forming the pelvic floor, the pelvic diaphragm consist of the coccygeus and levator ani muscles and their associated fascia. Making up the larger portion of the pelvic floor is the levator ani, which is made up of three parts: the puborectalis, the pubococcygeus, and the iliococcygeus. The puborectalis forms a sling around the posterior aspect of the anorectal junction and aids in retaining fecal continence. The levator ani function together to support the viscera with tonic contraction and to aid in forced expiration, among other activities, with active contraction. Relaxation of the levator ani occurs for urination and defecation to occur.
The perineum, which includes the anus and external genitalia, and has additional muscles associated with the external genitalia. Such muscles can be found within the pelvic cavity and include the ischiocavernosus and bulbospongiosus muscles. The ischiocavernosus muscle acts to compress the corpus cavernosum. The bulbospongiosus muscle has different actions in males and females. In males, the bulbospongiosus muscle acts to compress the bulb of the penis and also compresses the spongey urethra. In females, the bulbospongiosus muscle acts to compress the vestibular bulb and constrict the vaginal orifice.
There are several ligaments associated with the pelvis. Females have a ligament called the suspensory ligament of the ovary that is a fold of peritoneum through which the ovarian vessels, lymphatics, and nerves pass to cross the pelvic brim. To an extent, the suspensory ligament is continuous with the broad ligament. The broad ligament serves to anchor the uterus in place, extending from the uterus to the pelvic floor and the walls of the pelvis. Another ligament that serves to anchor the uterus is the cardinal ligament which maintains the anteverted position of the uterus. During pregnancy, the round ligament maintains the anteverted uterine position rather than the cardinal ligament.
A. Robinson
Sources:
Moore, Dalley, Agur: Clinically Oriented Anatomy. 6th ed. Baltimore: Lippincott Williams & Wilkins, 2010.