The liver is the largest gland in the body and the second largest organ (second to the skin). Among the liver’s myriad of functions are metabolic, vascular, and secretory functions. Functionally and positionally, the liver is intimately associated with the pancreas, the hepatic portal system, and the biliary tract. This intimate relationship is evidenced by the several impressions, fossa, and fissures found on the visceral surface of the liver. Some of these include an impression from the inferior vena cava along with a fossa for the gallbladder, and fossa for the porta hepatis. Making it very easy to distinguish from the visceral surface, the diaphragmatic surface of the liver is smooth due to the lack of such associations.

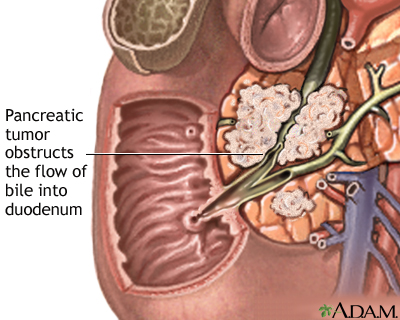
The bile duct joins with the main pancreatic duct to form the hepatopancreatic ampulla, also called the ampulla of Vater, which empties into the descending part (2nd part) of the duodenum. Around the most distal portion of the hepatopancreatic ampulla is a thickened, circular muscle called the sphincter of the bile duct, or commonly called the sphincter of Oddi. The spincter of the bile duct is found at the major duodenal papillae where the hepatopancreatic ampulla empties into the descending duodenum. Pancreatic cancer or gallstones can result in blockage of the bile duct, causing bile to build up within the liver. Temporary relief from blockage due to pancreatic tumors or pancreatic carcinoma can be achieved by insertion of a stent, an endoscopic procedure. Pancreatic cancer is typically not discovered until it is in late stages due to being asymptomatic during early stages and due to not being in an easily palpated location. Diabetes, smoking, and pancreatitis are major pancreatic cancer risk factors.
The cadaver that my group has been dissecting has an enlarged liver, known as hepatomegaly. This could be due to a rise in central venous pressure or diseases that cause hepatic engorgement. The liver becomes engorged with blood with an increase in central venous pressure, as associated with chronic contrictictive pericarditis, because of the large amount of blood that passes through the liver before entering the heart. Constrictive pericarditis is caused by the thickening of the pericardium which in turn causes restricted movement of the heart. Due to the restricted movement of the heart, the chambers do not fill with enough blood and blood becomes congested in areas such as the liver. A supporting factor for pericarditis affecting our cadaver is the white, flaky substance found covering the myocardium and the great vessels deep to the pericardium. This substance could have been due to the large amount of fibrin, which causes the pericardium to thicken in cases of pericarditis, which formed a fibrous exudate (protein-rich fluid that collects in a space) within the pericardium.
Other causes of hepatomegaly include (but are not limited to) viral hepatitis, primary hepatic tumors (hepatocellular carcinoma), secondary liver tumors (metastatic carcinoma), and common bile duct stones. Hepatitis uses hepatocytes (liver cells) as host cells for viral reproduction. The viral replication sparks the infiltration of lymphocytes into the affected areas in an effort to fight off the virus, causing inflammation. Chemicals released by the lymphocytes can damage the hepatovytes, causing cell death in some cases. During a physical the liver is palpated and if hepatomegaly is indicated, so is presence of tenderness. Hepatomegaly with tenderness indicates hepatomegaly caused by hepatitis or congestive heart failure. Another cause of hepatomegaly, liver metastases, are due to cancer of the breast, colon, esophagus, pancreas, lung, stomach, or melanoma. This is due to the cancer spreading from organs that drain directly into the liver by means of the portal system and cancer cells spreading from the thorax due to lymph vessel drainage.
The cadaver that my group has been dissecting also has gallstones. One gallstone is readily palpated at a size intermediate of a BB and a marble. Gallstones can be of two types: cholesterol stones or pigment stones. Cholesterol stones represent the majority of gallstones at around 80% of cases. Typically smaller and darker in color than cholesterol stones, pigment stones are made up of bilirubin. Risk factors for developing gallstones include high cholesterol and, once again, diabetes.Bile is produced and released by the liver. Hepatocytes, liver cells, produce bile from products of hemoglobin catabolism. The liver releases the bile from intrahepatic bile ducts into the left and right hepatic ducts which converge to form a common bile duct. Bile travels through the cystic duct to be stored in the gallbladder until it is needed. Following ingestion of food, bile is released into the common bile duct and into the duodenum, where it emulsifies ingested fats. Obstruction of the bile duct is typically indicated by light-colored, white, or clay-colored stool and typically results from gallstones or tumors.
A. Robinson
Sources:
http://home.comcast.net/~wnor/liver.htmSources:
Moore, Dalley, Agur: Clinically Oriented Anatomy. 6th ed. Baltimore: Lippincott Williams & Wilkins, 2010.
http://www.wrongdiagnosis.com/h/hepatitis_a/book-diseases-4a.htm
http://www.nlm.nih.gov/medlineplus/ency/presentations/100199_2.htm
http://library.med.utah.edu/WebPath/INFLHTML/INFL014.html
http://www.umm.edu/ency/article/003275.htm
http://www.patient.co.uk/doctor/Hepatomegaly.htm
http://www.gallstones.com/
http://api.ning.com/files/AllAboutHepatomegaly.pdf
http://www.pegassist.com/hepatitis-c-education/how-does-hepatitis-c-affect-my-liver.aspx


That was very interesting and informative. One of the most interesting aspects of this blog was the differentiation between the two types of gallstones (cholesterol & pigment). So to follow this up I thought you might be interested in a summary of the molecular mechanisms that are responsible for the formation of the cholesterol type gallstones. Obviously, this is NOT an additional pathology, but it shows the link between the formation and the results after formation.
ReplyDeleteEssentially, the formation of cholesterol is partially mediated by the CCK-AR gene. This abbreviation is for cholecystokinin-A receptor. This is a G-coupled receptor that is responsible for the direct modulation of Cholesterol. In essence, this gene can be upregulated to such as extent that cholesterol “clusters” can form; often in the gallbladder. Therefore, it is possible that upregulation of this gene lead to the formation of gallstones in our cadaver.
Reference:
Miyasaka K, Takata Y, Funakoshi A. Association of cholecystokinin A receptor gene polymorphism with cholelithiasis and the molecular mechanisms of this polymorphism. .Journal of Gastroenterology. 2002. 37. 102-6.